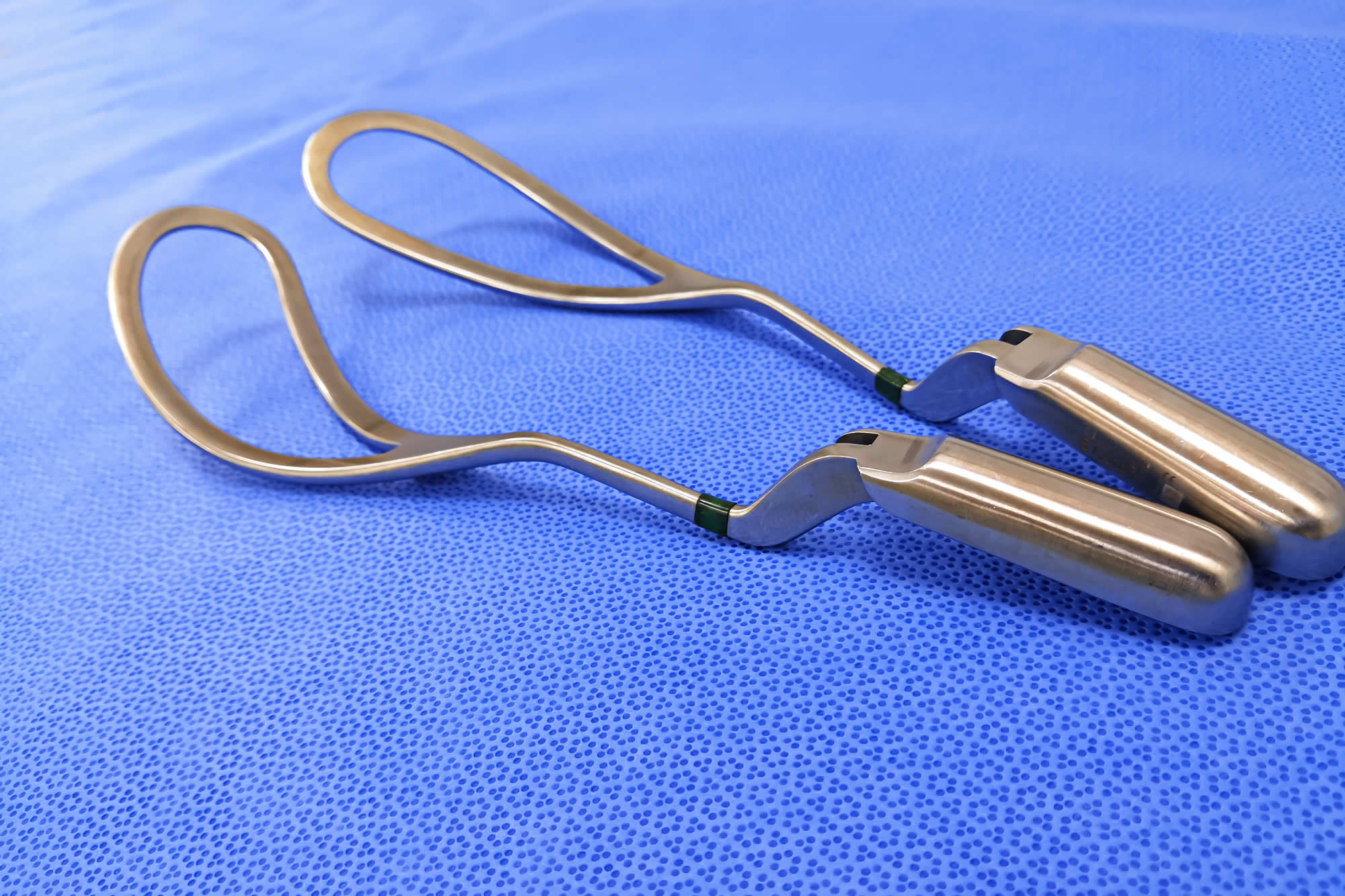
According to a recent analysis, the rate of severe and enduring injuries among Canadian mothers due to the utilization of forceps and vacuum during childbirth remains significantly high, urging immediate and concerted action to alleviate the situation. The paper, published in the medical journal BMJ, highlights Canada’s position with the highest maternal trauma rate compared to 24 other high-income countries, with a troubling 16 percent injury rate during forceps- and vacuum-assisted deliveries, as opposed to the 5 percent average for the cohort.
The study underscores the prevalence of obstetric anal sphincter injuries, a common consequence of forceps- and vacuum-assisted deliveries, affecting one in four attempted forceps deliveries and one in eight attempted vacuum deliveries in Canada. The long-term repercussions of these injuries can range from pelvic pain and sexual dysfunction to fecal and anal incontinence, significantly impacting the social, psychological, and physical well-being of affected mothers.
Laura Ralph, who experienced traumatic childbirth involving forceps, shared her emotional journey of enduring both physical and mental health challenges long after the birth of her son. Her involvement in the BMJ paper as a patient partner aimed to shed light on the often unspoken struggles faced by women post-childbirth, emphasizing the necessity for improved support and preventative measures.
Comparatively, countries such as the Netherlands, Finland, and Sweden, having abandoned the use of forceps entirely due to concerns over maternal trauma, have achieved zero percent injury rates. While some experts assert the safety of forceps and vacuum in trained hands, the call for more proactive approaches to childbirth, including enhanced education on alternatives like C-sections and episiotomy, has gained momentum.
The discourse around the efficacy of episiotomy, though previously contentious, has resurfaced as data indicates a potential role in preventing severe perineal tears during operative vaginal delivery. Advocates emphasize the need to facilitate open discussions on pelvic floor health and provide comprehensive pre-birth care to empower expectant mothers. However, caution is advised in making direct comparisons between countries, considering the complexity of childbirth practices and healthcare systems. Dr. Amanda Black, president of the Society of Obstetricians and Gynecologists of Canada, stressed the significance of addressing concerns over the escalating rates of obstetric sphincter injuries, urging a collaborative effort towards improved maternal healthcare practices in the country.